Table of Contents
Introduction
Spermatogenesis is the process of sperm cell formation and development. It occurs in the testes of males, and it is regulated by a complex interplay of hormones, including testosterone and follicle-stimulating hormone (FSH). This chapter will discuss the process of it, focusing on the different phases of it, the hormonal regulation of it, and the disorders that can occur as a result of hormonal imbalances.
Phases of Spermatogenesis
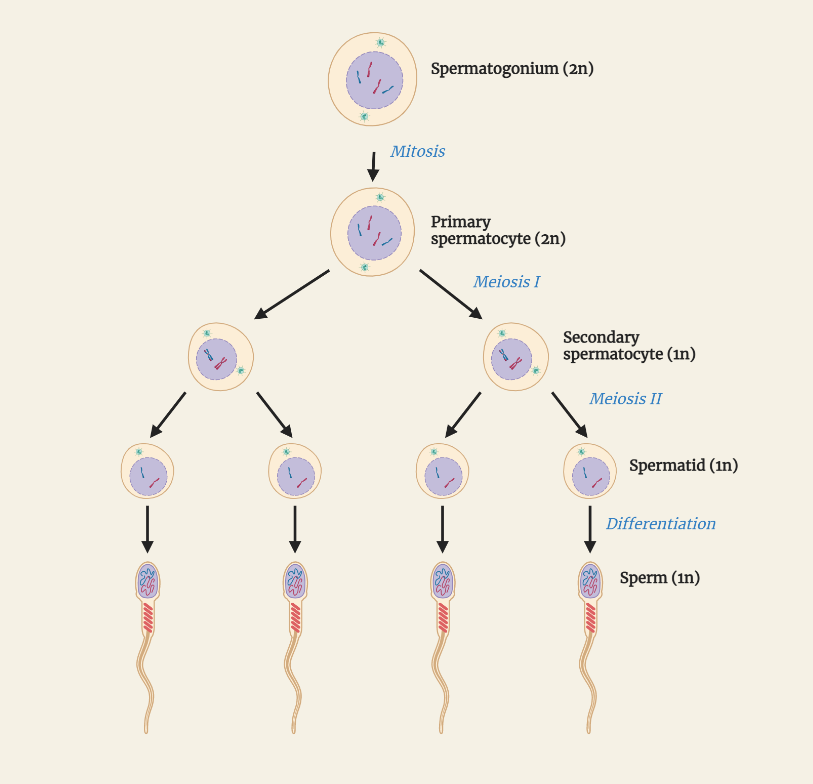
It is divided into four main phases: the mitotic phase, the meiotic phase, the morphological maturation phase, and the maturation phase.
Mitotic phase:
This phase begins in the outermost layer of the testes, the Seminiferous epithelium. It is characterized by the rapid proliferation of spermatogonial stem cells. These cells divide mitotically, forming primary spermatocytes.
Meiotic phase:
This phase begins when the primary spermatocytes reach the basement membrane. It is characterized by the first meiotic division, which leads to the formation of secondary spermatocytes. The second meiotic division then leads to the formation of spermatids.
Morphological maturation phase:
This phase begins after the formation of spermatids. It is characterized by the differentiation and morphological maturation of spermatids into spermatozoa. This includes the formation of the flagellum, the acrosome, and the midpiece.
Maturation phase:
This phase begins after the morphological maturation of spermatozoa. It is characterized by the maturation of spermatozoa in the epididymis, where they acquire the ability to fertilize an egg.
Hormonal Regulation of Spermatogenesis
It is regulated by a complex interplay of hormones, including testosterone and FSH. Testosterone, produced by the Leydig cells in the testes, is the primary hormone responsible for the regulation of spermatogenesis. It stimulates the proliferation of spermatogonial stem cells and the differentiation of spermatocytes into spermatozoa. FSH, produced by the pituitary gland, regulates the mitotic phase of spermatogenesis by stimulating the proliferation of spermatogonial stem cells.
Disorders
Hormonal imbalances can lead to a wide range of disorders that affect spermatogenesis. These include:
Klinefelter’s syndrome:
a genetic disorder characterized by an extra X chromosome, leading to reduced testosterone levels and infertility.
Hypogonadism:
a condition characterized by reduced testosterone levels, leading to reduced spermatogenesis and infertility.
Varicocele:
an enlargement of the veins in the testes, which can lead to reduced spermatogenesis and infertility.
Conclusion
Spermatogenesis is a complex process that is regulated by a delicate balance of hormones, including testosterone and FSH. Understanding the different phases of spermatogenesis, the hormonal regulation of it, and the disorders that can occur as a result of hormonal imbalances is essential for understanding male fertility and reproductive health. Additionally, studying spermatogenesis also allows us to understand the functioning of the male reproductive system and any abnormalities that may occur.